Throat (Oropharyngeal) cancer incidence is on the rise….
And now commonly affects a different demographic than you would naturally expect: young males with minimal exposure to tobacco or alcohol. It used to be that squamous cell carcinoma (the type of cancer that makes up > 90% of throat cancers) was associated with older males who drank and smoked excessively. Not anymore.
Human papilloma virus (HPV) has changed everything and now accounts for 40 – 90% of all throat cancers. This is the same kind of tumor that Michael Douglas developed. The scary thing is that the overall incidence of head and neck cancer has gone down, whereas the incidence of HPV-associated throat cancer has risen by 225%. It is estimated that there will be more HPV-associated throat cancer than cervical cancer by 2020!
What has changed? People are pointing at sexual histories. The new cancer patient doesn’t drink or smoke excessively but their histories suggest increased numbers of sexual encounters, both vaginal and oral. It is also associated with exposure to marijuana and has been shown to be more likely in husbands who have wives with cervical cancer. 85% of us get HPV infections at some point in our lives. There are over 120 HPV subtypes that can infect us. An extremely small percentage of us will go on to develop cancer many years later. Subtypes 16 and 18 are the most likely types to cause both cervical and throat cancer.
HPV-Related Tumors
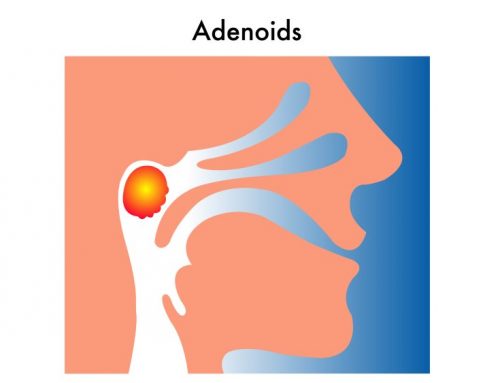
Patients with HPV-related tumors also present differently. The average age of presentation is in the 5th or 6th decade. Their tumors tend to be smaller than non-HPV tumors; however, they are more likely to present with early spread to the neck lymph nodes. Tumors arise from either the tonsil or the back of the tongue (base of tongue).
Overall, patients with HPV-related tumors have much higher survival rates than those with HPV-negative tumors. We are still learning how best to treat HPV-related squamous cell carcinoma, as good outcomes are being reported with chemoradiation approaches as well as up-front surgical approaches. The primary objective then becomes minimizing complications and morbidity from these therapies. For example, many studies are underway to see if less radiation to HPV-positive tumors and, therefore less delivered toxicity, will result in the same overall survival. Similarly, in select cases, surgical techniques have evolved that sometimes spare the need for any additional (adjuvant) therapies.
Get Vaccinated?
What else you do you need to know? This is not a contagious cancer as the HPV exposure occurred well before (i.e., many years) transformation into malignancy. While it is not helpful for an adult to get vaccinated, it is probably very smart to get both boys and girls vaccinated before they become sexually active. Vaccination is recommended for all adolescents and young adults (male and female)—ages 9 to 25, ideally prior to onset of sexual activity. The vaccine provides protection against the 4 strains of HPV most associated with cervical and throat cancer, including HPV-16.




Leave A Comment